Da Vinci Robotic Surgical System: Early Experience from Pakistan
By Harris Hassan Qureshi, Rehan Mohsin, Naveed Ahmed Mahar, Riaz Ahmed Laghari, Mushtaq Hussain, Altaf HashmiAffiliations
doi: 10.29271/jcpsp.2024.04.489ABSTRACT
Objective: To determine the outcomes of robotic surgeries using the Da Vinci robotic surgical system (DVSS) at Pakistan’s largest urological tertiary healthcare system.
Study Design: Descriptive study.
Place and Duration of the Study: Department of Minimally Invasive and Robotic Surgery, Division of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan, from March 2017 to December 2021.
Methodology: Hospital records of patients who underwent robotic urological surgeries were assessed for their outcomes in terms of blood loss, mortality, system malfunction, and conversion to open surgery. Descriptive statistics were determined.
Results: A total of 550 procedures were performed. The mean age recorded was 39.58±16.83 years. The mean blood loss recorded was 255.611±353.57 ml; there were 3 cases of malfunction. Forty cases were converted to open surgery, and the mortality rate was 1.1%.
Conclusion: Minimally invasive surgical techniques have high precision, fewer complications, and lower morbidity rates. Using DVSS for surgical interventions is both effective and safe.
Key Words: Minimally invasive surgery, Da Vinci robotic surgical system, Robotic surgery.
INTRODUCTION
The da vinci robotic surgical System (DVSS) has been widely used for urologic procedures since it was first introduced in 1999 for cardiac procedures. Intuitive Surgical data indicates that around two million operations were carried out in 2013.1-3 It is the surgical robot that has been recognised and investigated the most. It works on a master-slave telemanipulation system in which the master uses a computer-video console to direct three or four robotic surgical arms. The DVSS may cause significantly less blood loss, fewer complications, less postoperative discomfort, a shorter length of hospital stay, and quicker recovery than traditional open surgical techniques. These benefits have sparked a great deal of attention among medical professionals and patients.4 Given the Da Vinci System's early introduction and rising distribution, as well as its high capital and running expenses, a clinical and economic study is needed to assist decision-makers on its procurement and eventual usage.5
Despite the usual lack of long-term curative treatment outcomes and the greater cost of robotic treatments compared to other forms of surgery, robotic technology is commonly used in oncologic surgery, with documented short-term benefits.6 Numerous studies have shown the effectiveness and safety of robotic procedures for treating a range of ailments, with results comparable to those of laparoscopic surgery.7-12 No research, as far as the authors are aware, has suggested a comprehensive analysis based on the actions of many departments inside a single institution. The use of robots during surgery has reduced a number of drawbacks, such as setup costs and the need for surgical training. Robotic surgery will eventually replace open and laparoscopic surgery globally. As technology advances, robots are becoming increasingly precise, making them ideal for a wide range of applications within the medical sector. The objective of this research was to assess the efficacy of the robotic procedures conducted at the Sindh Institute of Urology and Transplantation, Karachi, as well as to determine the advantages and potential drawbacks connected with these procedures.
METHODOLOGY
This study was conducted at the Department of Urology, Sindh Institute of Urology and Transplantation, after obtaining approval from the Ethics Review Committee of the hospital. The data of patients who underwent robotic surgery between 2017 and 2021 was fetched from the department’s medical record. Patients who had no previous history of open abdominal surgery, American Society of Anaesthetist (ASA) level-I status and no evidence of system diseases were included in this study. Patients with multiple comorbid and ASA status level-II or above were excluded from this study.
All the data regarding basic demographics, surgical procedures, and outcomes in terms of blood loss, mortality, system malfunction and conversion to open surgery were recorded and analysed using IBM SPSS 23. For categorical variables, frequencies and percentages were calculated and for numerical data, mean and SD were calculated.
RESULTS
A total number of 550 surgeries were performed from 2017 to 2021. Majority of the patients were males accounting for 346 (62.9%) and 204 (37.1%) were females. The mean age of the patients was 39.58±16.83 years and the mean BMI was 30.13±3.52 kg/m2.
Out of 550 cases, majority of 137 (24.9%) were performed in the first year (2017) of robot installation, 117 (21.3%) cases in 2018, 61 (11.1%) cases in 2019, 119 (21.6%) in 2020, and 116 (21.1%) cases in 2021.
The mean blood loss was 255.611±353.57 ml, and a total of 3 cases of system malfunction were observed. Forty-two cases were converted to open surgery. Postoperative complications were observed among 2.7% of patients and 97.3% of patients remained complication-free. Majority of the complications were gastrointestinal tract-related mainly ileus. The mortality rate was 1.1%. The total no. of procedures performed is shown in Figure 1. Radical nephrectomy and pyeloplasty were the most frequent procedures performed. Table I demonstrates year-wise distribution of the performed procedures.
Table I: Year-wise distribution of different procedures.|
Procedure |
2017 |
2018 |
2019 |
2020 |
2021 |
Total |
|
Simple nephrectomy |
65 |
3 |
0 |
4 |
4 |
76 |
|
47.40% |
2.60% |
0.00% |
3.40% |
3.40% |
13.80% |
|
|
Pyeloplasty+DJ |
25 |
43 |
25 |
21 |
38 |
152 |
|
18.20% |
36.80% |
41.00% |
17.60% |
32.80% |
27.60% |
|
|
Ureteric reimplant |
0 |
0 |
1 |
9 |
4 |
14 |
|
0.00% |
0.00% |
1.60% |
7.60% |
3.40% |
2.50% |
|
|
Pyelolithotomy |
7 |
5 |
0 |
6 |
3 |
21 |
|
5.10% |
4.30% |
0.00% |
5.00% |
2.60% |
3.80% |
|
|
Pyelolithotomy+pyeloplasty+DJ |
1 |
1 |
4 |
4 |
2 |
12 |
|
0.70% |
0.90% |
6.60% |
3.40% |
1.70% |
2.20% |
|
|
Cystolithotomy |
0 |
0 |
0 |
1 |
0 |
1 |
|
0.00% |
0.00% |
0.00% |
0.80% |
0.00% |
0.20% |
|
|
Ureterolithotomy |
1 |
2 |
3 |
8 |
3 |
17 |
|
0.70% |
1.70% |
4.90% |
6.70% |
2.60% |
3.10% |
|
|
Simple prostectomy |
0 |
0 |
0 |
3 |
7 |
10 |
|
0.00% |
0.00% |
0.00% |
2.50% |
6.00% |
1.80% |
|
|
Radical prostectomy+LND |
7 |
4 |
3 |
4 |
6 |
24 |
|
5.10% |
3.40% |
4.90% |
3.40% |
5.20% |
4.40% |
|
|
Nephrolithotomy |
0 |
0 |
0 |
2 |
0 |
2 |
|
0.00% |
0.00% |
0.00% |
1.70% |
0.00% |
0.40% |
|
|
Cyst marsupilisation |
2 |
1 |
0 |
1 |
1 |
5 |
|
1.50% |
0.90% |
0.00% |
0.80% |
0.90% |
0.90% |
|
|
Radical cystectomy+ileal conduit |
2 |
8 |
1 |
9 |
5 |
25 |
|
1.50% |
6.80% |
1.60% |
7.60% |
4.30% |
4.50% |
|
|
Adrenalectomy |
1 |
3 |
2 |
4 |
5 |
15 |
|
0.70% |
2.60% |
3.30% |
3.40% |
4.30% |
2.70% |
|
|
Radical nephrectomy |
21 |
31 |
17 |
30 |
27 |
126 |
|
15.30% |
26.50% |
27.90% |
25.20% |
23.30% |
22.90% |
|
|
Partial nephrectomy |
4 |
16 |
3 |
9 |
9 |
41 |
|
2.90% |
13.70% |
4.90% |
7.60% |
7.80% |
7.50% |
|
|
Renal cyst biopsy and deeroofing |
0 |
0 |
1 |
1 |
0 |
2 |
|
0.00% |
0.00% |
1.60% |
0.80% |
0.00% |
0.40% |
|
|
Partial cystectomy |
0 |
0 |
1 |
1 |
0 |
2 |
|
0.00% |
0.00% |
1.60% |
0.80% |
0.00% |
0.40% |
|
|
Radical cystectomy+continent diversion |
0 |
0 |
0 |
2 |
1 |
3 |
|
0.00% |
0.00% |
0.00% |
1.70% |
0.90% |
0.50% |
|
|
Bilateral ureterostomies |
0 |
0 |
0 |
0 |
1 |
1 |
|
0.00% |
0.00% |
0.00% |
0.00% |
0.90% |
0.20% |
|
|
VVF repair |
1 |
0 |
0 |
0 |
0 |
1 |
|
0.70% |
0.00% |
0.00% |
0.00% |
0.00% |
0.20% |
|
|
Total |
137 |
117 |
61 |
119 |
116 |
550 |
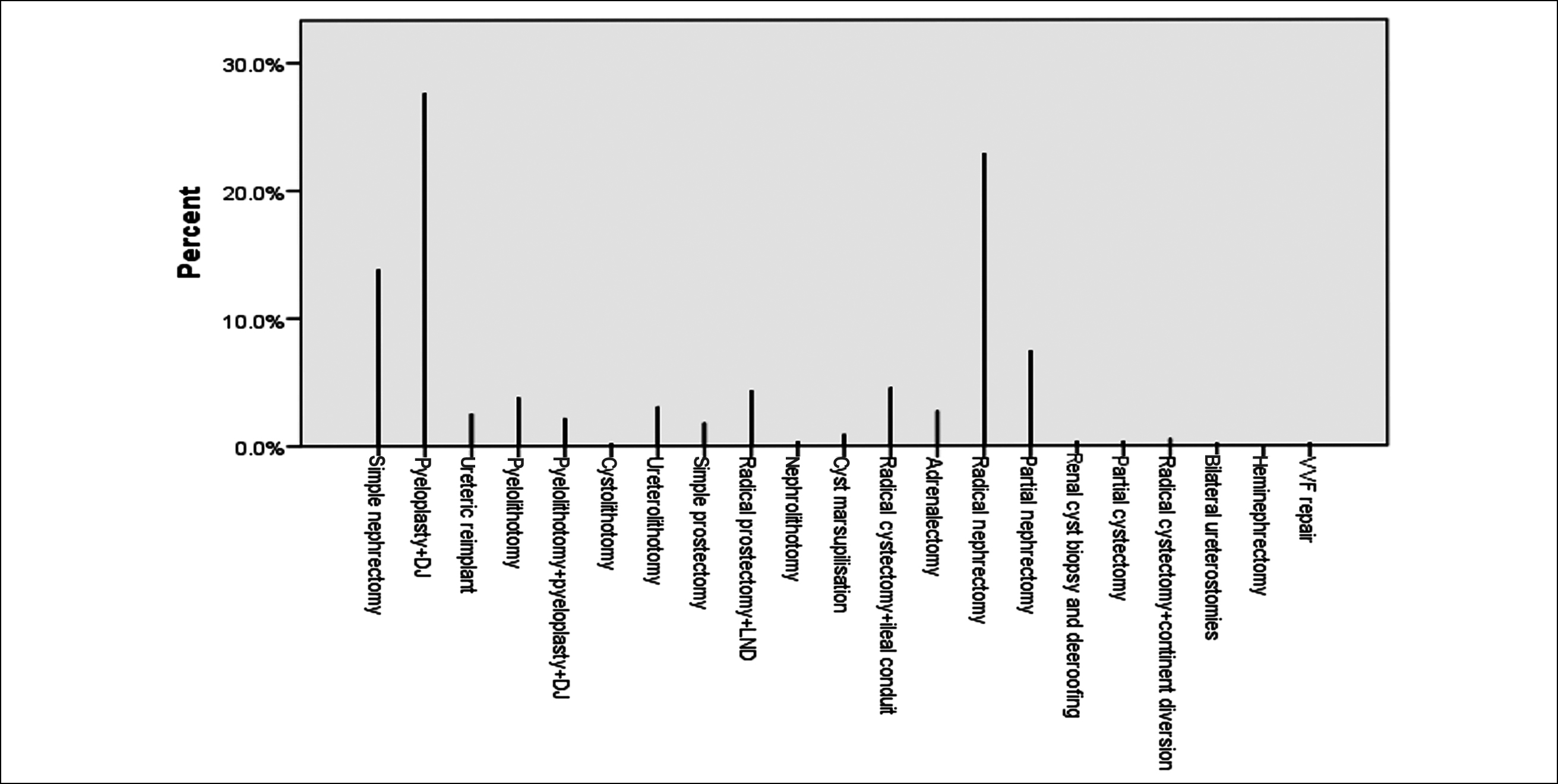 Figure 1: Graph showing total number and frequency of different procedures that were performed.
Figure 1: Graph showing total number and frequency of different procedures that were performed.
DISCUSSION
Over the previous two decades, robotic surgery and minimally invasive surgery have both significantly advanced to the point where they are now some of the most widely used forms of surgical procedure. Robotic surgery has evolved significantly, emerging as one of the most widely adopted surgical approaches. It offers a range of compelling benefits for patients, including diminished postoperative discomfort, shortened hospitalisation periods, accelerated recovery rates, and minimised incisions, all of which contribute to an overall improved patient experience. Particularly advantageous for intricate procedures within confined anatomical spaces, robotic surgery provides surgeons with a magnified three-dimensional perspective of the operative area, enabling precise and informed decision-making.
In a comprehensive study conducted by Steffens et al. a meticulous comparison was made among various surgical techniques, including robotics, laparoscopy, and open surgery, to assess their respective outcomes.10 This investigation encompassed a dataset consisting of 184 patients who had undergone urological procedures via robotic means. Notably, the average age of these patients was 65 years. The findings of Steffens et al. revealed a remarkably low complication rate of 1.6%, and thankfully, there were no reported mortalities. Furthermore, the typical length of hospital stay for these patients was around 2±1 days. In this study, the patient cohort exhibited a different demographic profile, with a mean age of 39.58±16.83 years. In this group, complications were observed in 2.7% of patients. It is noteworthy that the majority of these complications were self-limiting and did not lead to severe, long-term consequences. This study also observed a mortality rate of 1.1% among the patients. These findings highlight the importance of considering patient demographics and surgical techniques when interpreting outcomes and making clinical decisions in the field of urology.10
In a distinct research study, Hussein et al. shared their experiences in transitioning from the da Vinci robotic system to the Versius robotic system, along with the outcomes of their initial 100 cases. The median age of the patients in their study was 42 years, with an interquartile range (IQR) spanning from 26 to 56. A significant proportion, approximately 75%, of their surgical procedures were conducted in the upper urinary tract, with a predominant focus on benign conditions, accounting for approximately 83% of cases. Their findings indicated that system failure occurred in 2% of cases, and the conversion to open surgery in 6% of instances. Furthermore, Hussein and colleagues reported a complication rate of 8%. In this study’s patient cohort, the majority of surgeries also involved the upper urinary tract, with pyeloplasty being the most frequently performed procedure, accounting for 27.6% of cases, followed by radical nephrectomy at 22.9%. Interestingly, notable differences in the results compared to Hussein et al.'s findings were observed. Specifically, the rates of system failure and complications in this study were substantially lower, with system failures occurring in only 0.5% of cases and complications observed in 2.7% of cases. However, it is worth noting that the conversion rate to open surgery was slightly higher at 7.4%.13
The potential benefits associated with robotic-assisted lapa-roscopic surgery include reduced hospitalisation duration, minimised blood loss, and diminished postoperative pain. In a study conducted by Kim et al., involving a series of 157 robotic-assisted laparoscopic prostatectomies, a median blood loss of 100 millilitres was documented.14 Agarwal et al. similarly documented a median blood loss of 200 millilitres, along with an associated complication rate of 8.1%.15 In another investigation, a median blood loss of 50 millilitres was reported. Notably, in this study, the mean blood loss averaged at 255.611 millilitres with a standard deviation of 353.57 millilitres. This figure aligns closely with the data presented in the existing literature.16
A notable constraint of this research lies in its retrospective nature. Gathering data after the events have transpired introduces the potential for bias. Moreover, this study is confined to foundational cases within the initial learning phase, potentially falling short in capturing the nuances of intricate scenarios. Consequently, the transferability of these findings to more complex situations might be challenged, somewhat circumscribing the study's comprehensive applicability. Given these inherent limitations, it is prudent to approach the study's outcomes with a measured perspective. Vigilance is advised, and there arises a need for further comprehensive investigation to corroborate the findings across a broader spectrum of circumstances. Such endeavours would enhance the reliability and depth of the study's conclusion, fortifying the groundwork for a more extensive understanding of the subject matter.
CONCLUSION
Robotic surgery may be considered a risk-free substitute for traditional surgery due to the wide array of advantages it provides, such as improved surgical accuracy, less patient pain and discomfort, a shorter hospital stay, and fewer postoperative complications.
ETHICAL APPROVAL:
Ethical approval for this research project was obtained from the institute’s ethics review committee [SIUT-ERC-2022/ A-396]. The approval ensures that this study adheres to ethical standards and guidelines, prioritising the well-being and rights of the participants involved in the research process.
PATIENTS’ CONSENT:
In light of the logistical challenges associated with obtaining individual informed consent for this study, which involves the use of pre-existing data, the authors hereby declare their unwavering commitment to upholding ethical standards and respecting patient autonomy throughout the research process. Patient confidentiality was maintained throughout.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
HHQ: Concept, study design, and drafting the manuscript.
RM: Concept, drafting the manuscript, and critical review of data.
NAM: Study design, data analysis and acquisition, drafting manuscript, and literature review.
RAL: Data acquisition and literature search.
MH: Data acquisition, literature search, and literature review.
AH: Critical analysis of the manuscript and final approval.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Barbash GI, Glied SA. New technology and health care costs--the case of robot-assisted surgery. N Engl J Med 2010; 363(8):701-4. doi: 10.1056/NEJMp1006602.
- Can Ö, Gedik MA, Köylüoğlu N, Yangal HS, Aysun Ö. Sağlıkta Yapay Zeka ve Uygulamaları: Akademisyen Kitabevi; 2021; 426. doi: 10.37609/akya.117.
- Almarzouq A, Hu J, Noureldin YA, Yin A, Anidjar M, Bladou F, et al. Are basic robotic surgical skills transferable from the simulator to the operating room? A randomized, prospective, educational study. Can Urol Assoc J 2020; 14(12): 416-22. doi: 10.5489/cuaj.6460.
- MacCraith E, Forde JC, Davis NF. Robotic simulation training for urological trainees: A comprehensive review on cost, merits and challenges. J Robot Surg 2019; 13(3):371-7. doi:10.1007/s11701-019-00934-1.
- Hechenbleikner EM, Jacob BP. Medicolegal issues in robotic surgery. Robotic-assisted minim invasive surg 2018; 27-34. doi:10.1007/978-3-319-96866-7_4.
- Almujalhem A, Rha KH. Surgical robotic systems: What we have now? A urological perspective. BJUI Compass 2020; 1(5):152-9. doi: 10.1002/bco2.31.
- Farinha R, Puliatti S, Mazzone E, Amato M, Rosiello G, Yadav S, et al. Potential contenders for the leadership in robotic surgery. J Endourol 2022; 36(3):317-6. doi: 10. 1089/end.2021.0321.
- Azhar RA, Elkoushy MA, Aldousari S. Robot-assisted urological surgery in the Middle East: Where are we and how far can we go? Arab J Urol 2019; 17(2):106-13. doi: 10.1080/ 2090598X.2019.1601003.
- Petz W, Borin S, Fumagalli Romario U. Updates on robotic CME for right colon cancer: A qualitative systematic review. J Pers Med 2021; 11(6):550. doi: 10.3390/jpm11060550.
- Steffens D, McBride KE, Hirst N, Solomon MJ, Anderson T, Thanigasalam R, et al. Surgical outcomes and cost analysis of a multi-specialty robotic-assisted surgery caseload in the Australian public health system. J Robot Surg 2023; 17(5):2237-45. doi: 10.1007/s11701-023-01643-6.
- Koh DH, Jang WS, Park JW, Ham WS, Han WK, Rha KH, et al. Efficacy and safety of robotic procedures performed using the da vinci robotic surgical system at a single institute in Korea: Experience with 10000 cases. Yonsei Med J 2018; 59(8):975-81. doi: 10.3349/ymj.2018.59.8.975.
- He S, Weng Y, Jiang Y. Robot-assisted radical resection in prostate cancer comparative assessment with conventional laparoscopic prostatectomy: A retrospective comparative cohort study with single-center experience. Transl Androl Urol 2022; 11(12):1729-34. doi: 10.21037/tau-22-739.
- Hussein AA, Mohsin R, Qureshi H, Leghari R, Jing Z, Ramahi YO, et al. Transition from da Vinci to versius robotic surgical system: Initial experience and outcomes of over 100 consecutive procedures. J Robot Surg 2023; 17(2):419-26. doi: 10.1007/s11701-022-01422-9.
- Kim JE, Kaldany A, Lichtbroun B, Singer EA, Jang TL, Ghodoussipour S, et al. Single-port robotic radical prostatectomy: Short-term outcomes and learning curve. J Endourol 2022; 36(10):1285-9. doi: 10.1089/end.2021.0885.
- Agarwal DK, Sharma V, Toussi A, Viers BR, Tollefson MK, Gettman MT, et al. Initial experience with da Vinci single-port robot-assisted radical prostatectomies. Eur Urol 2020; 77(3):373-9. doi: 10.1016/j.eururo.2019.04.001.
- Moschovas MC, Bhat S, Rogers T, Onol F, Roof S, Mazzone E, et al. Technical modifications necessary to implement the da Vinci single-port robotic system. Eur Urol 2020; 78(3):415-23. doi: 10.1016/j.eururo.2020.01.005.